Hospital Capacity Units are a critical aspect of healthcare infrastructure, reflecting a hospital’s ability to provide care to patients at any given time. Understanding the factors that influence hospital capacity and the strategies employed to manage it is crucial for both healthcare professionals and the public alike. This article delves into the intricacies of hospital capacity units, shedding light on their significance in ensuring timely and effective patient care.
What Constitutes a Hospital Capacity Unit?
Contrary to a simple bed count, a hospital capacity unit is a multifaceted concept. It encompasses not only the physical number of beds but also the availability of trained personnel, specialized equipment, and essential resources like medications and blood products. A hospital capacity unit represents the confluence of these factors, signifying a hospital’s readiness to admit and treat patients effectively.
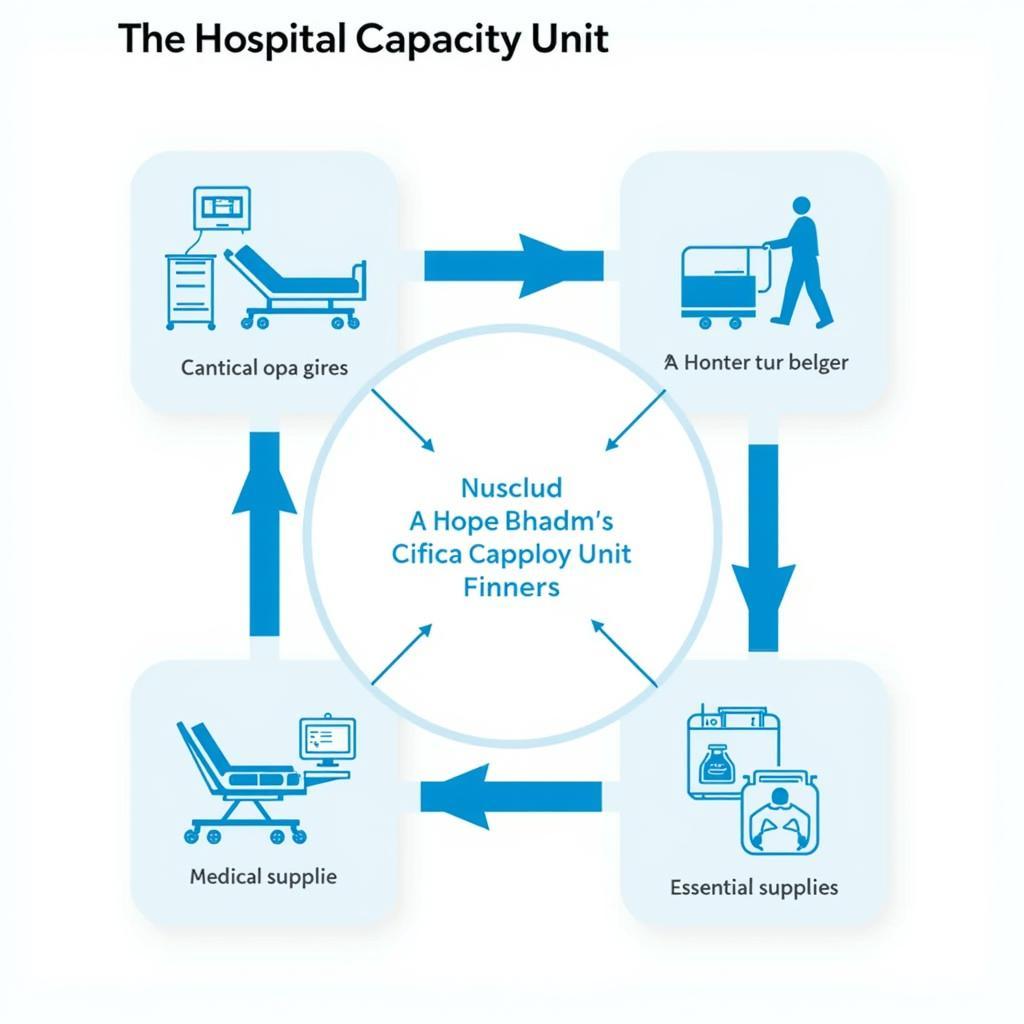 Key Components of a Hospital Capacity Unit
Key Components of a Hospital Capacity Unit
Factors Affecting Hospital Capacity
A myriad of factors can influence a hospital’s capacity.
- Seasonal Fluctuations: Influenza season, for instance, can strain hospital capacity due to a surge in respiratory illness cases.
- Natural Disasters: Events like earthquakes or hurricanes can lead to a sudden influx of trauma patients, overwhelming existing resources.
- Pandemics: Global health crises, like the recent COVID-19 pandemic, can severely impact hospital capacity, necessitating extraordinary measures to accommodate the surge in critically ill patients.
 Challenges to Maintaining Optimal Hospital Capacity
Challenges to Maintaining Optimal Hospital Capacity
Strategies for Managing Hospital Capacity
Hospitals employ various strategies to manage capacity effectively:
- Patient Flow Optimization: This involves streamlining patient admissions, discharges, and transfers to ensure beds are readily available for those in need.
- Staffing Flexibility: Hospitals often utilize flexible staffing models, adjusting nurse-to-patient ratios based on patient acuity and volume to ensure adequate coverage.
- Telehealth Integration: Leveraging telehealth technologies to provide remote consultations and monitoring can help manage capacity by reducing unnecessary hospital visits.
The Role of Technology in Optimizing Hospital Capacity Units
Technological advancements play a pivotal role in enhancing hospital capacity management. Electronic Health Records (EHRs) facilitate seamless information sharing, enabling efficient bed management and discharge planning. Predictive analytics tools can forecast patient volume, allowing hospitals to proactively allocate resources and staff accordingly.
The Importance of Community Collaboration
Effective hospital capacity management extends beyond the hospital walls. Collaboration with community healthcare providers, such as clinics and long-term care facilities, is essential. By coordinating care transitions and sharing patient information, hospitals can prevent unnecessary hospitalizations and optimize resource utilization across the continuum of care.
Conclusion
Hospital capacity units are fundamental to a well-functioning healthcare system. By understanding the factors influencing capacity and employing proactive management strategies, hospitals can ensure their ability to provide timely and effective care to all patients in need. As healthcare landscapes continue to evolve, embracing innovative solutions and fostering community partnerships will be paramount in optimizing hospital capacity units to meet the ever-changing needs of the communities they serve.
For those seeking information about specific hospital capacities, resources like the Scale Hospital database can provide valuable insights.
FAQs about Hospital Capacity Units
What is the difference between hospital capacity and occupancy?
Hospital capacity refers to the maximum number of patients a hospital can treat at a given time, considering available beds, staff, and resources. Occupancy, however, represents the actual number of patients currently hospitalized.
How can I find information about a specific hospital’s capacity?
Hospital capacity information is often available on their websites or through local health departments. You can also explore online resources like the Scale Hospital database for comprehensive insights.
How does hospital capacity impact patient care?
Optimal hospital capacity ensures timely access to care, reduced wait times, and adequate resources for effective treatment. When capacity is strained, patients may experience delays, limited bed availability, and potential compromises in care quality.
What steps can hospitals take to improve their capacity during emergencies?
During emergencies, hospitals can activate surge plans, which may involve canceling elective procedures, setting up temporary treatment areas, and requesting additional staff support from other facilities.
What is the role of the community in supporting hospital capacity?
The community plays a vital role by seeking care from appropriate settings like clinics for non-emergent needs, getting vaccinated to prevent preventable illnesses, and adhering to public health recommendations during outbreaks.